Quality Payment Program

Learn about the Centers for Medicaid & Medicare’s Quality Payment Program (QPP) and see how the CMS is reimbursing rheumatologists and other providers for services. In addition, see the definitions of standard QPP terms in the CMS QPP glossary.
The American College of Rheumatology’s RISE registry is building upon the latest technology to help you meet federal reporting requirements. Learn how RISE gives you the tools you need to succeed in an evolving federal reporting landscape.
Read the ACR’s latest comments to the CMS regarding the QPP.
Quality Payment Program Tracks
The QPP has three tracks to choose from, which allow you to participate based on your practice size, specialty, location, or patient population: MIPS, MVPs, and APMs.
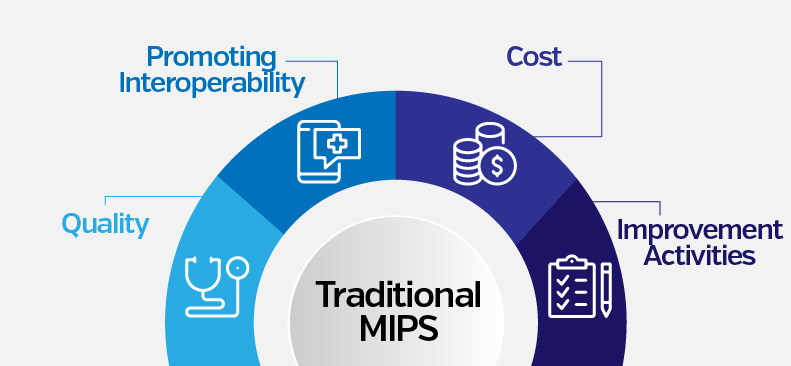
- MIPS evaluates four performance categories: Quality, Improvement Activities (IA), Promoting Interoperability (PI), and Cost. An eligible clinician’s performance score will determine if they receive a positive, negative, or neutral payment adjustment.
MIPS Resources
2025 Quality Measures in RISE
2026 QCDR Measures in RISE
2025 RISE Recommended Quality Measures
RISE Traditional MIPS & MIPS Value Pathways (MVPs) Toolkit
QPP Traditional MIPS Overview
QPP Resource Library
- MIPS Value Pathways (MVPs) are a subset of measures and activities that can be used to meet MIPS reporting requirements beginning in the 2023 performance year.
- The Advancing Rheumatology Patient Care MVP, created by the ACR and available through the RISE registry, offers rheumatology providers nine reportable quality measures that are highly relevant to rheumatology.
- The Advancing Rheumatology Patient Care MVP also focuses improvement activities on 11 options that rheumatology experts have vetted, rather than the 105 available through traditional MIPS.
- In addition to the traditional performance categories, MVPs also require practices to choose from two Population Health measures.
MVP Resources
2025 Quality Measures in RISE
2026 QCDR Measures in RISE
2025 RISE Recommended Quality Measures
Looking Forward to the Rheumatology MIPS Value Pathway
Advancing Rheumatology Patient Care MVP Toolkit
Video – MIPS Value Pathways: The Future of MIPS
QPP MIPS Value Pathways (MVP)
2025 QPP MVP Quality Measure Guide
- MACRA promotes the development of an eligible professional’s participation in Alternate Payment Models (APMs), which create a payment incentive program for qualifying participants.
- From 2019 through 2024, qualifying APM participants will receive a lump sum incentive payment equal to five percent of the prior year’s estimated aggregate expenditures under the fee schedule. Qualifying APM participants will not be subject to MIPS adjustments.
For inquiries and further deatils, please contact your APM administrator.
APM Resources
QPP Advanced APMs
QPP APMs Overview
QPP MIPS APMs Overview

